Exposure to ultraviolet (UV) rays from the sun can damage skin and increase risk of skin cancer. Too much sun exposure is also known to cause premature aging of the skin including wrinkles and sunspots, and could possibly cause a weakened immune system.
For people with diabetes, sun protection is even more important for multiple reasons. By following sun safety measures, you can minimize risks and enjoy the outdoors safely.
Keep reading to learn about why it is crucial to protect yourself from the sun and how to protect yourself best, especially when you have diabetes.
Type 2 diabetes and sun exposure
People with diabetes can experience slower healing due to elevated blood sugar levels. This can cause sunburns or other skin injuries to take longer to heal and also increases the risk of infection.
Certain medications used to treat diabetes can also make the skin more sensitive to sun, which can lead to an increased sunburn risk.
Additionally, neuropathy, or nerve damage – which is a complication some people with diabetes experience – might make sunburn detection difficult. Neuropathy can cause numbness, tingling or burning pain in the hands, feet and legs. This can also affect the skin, making it harder to feel the burning sensation that often comes with sunburn. Someone with neuropathy might not realize that they’ve been sunburned until the sunburn is severe.
The benefits of sun exposure
Sun exposure is not all bad, however. Sunlight exposure may play a positive role in blood sugar control through vitamin D production and circadian rhythm regulation.
Sunlight helps regulate the body’s natural sleep-wake cycle. Consistent exposure to sunlight, particularly in the morning, helps to synchronize our internal clock and keeps our sleep-wake schedule aligned with the natural day and night, promoting better sleep quality. Morning sunlight exposure can also boost daytime alertness and energy levels.
Studies suggest a link between low vitamin D and increased risk of type 2 diabetes, so getting some Vitamin D from the sun could help reduce the risk of developing type 2 diabetes.
Being safe in the sun and protecting your skin is crucial to reap the benefits without the risks.
Sun safety tips for people with diabetes
Sun awareness
- Seek shade whenever possible during peak sun hours of 10 am-4 pm.
- Try to plan outdoor activities for earlier or later in the day either before or after peak sun hours.
Skin protection
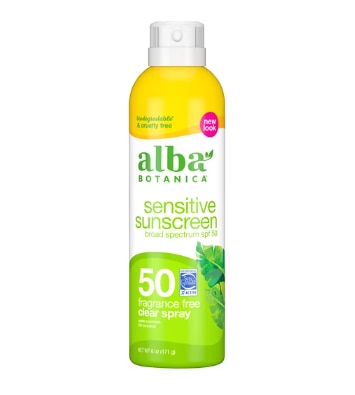
- Apply a broad-spectrum sunscreen with SPF 30 or higher liberally at least 15 minutes before going outside and reapply every two hours, especially after swimming or sweating.
- Apply sunscreen even on cloudy days.
- Consider wearing sun-protective clothing like long sleeves, pants, hats with brims, and sunglasses when outside in the direct sunlight.
- Look for clothes with a Ultraviolet Protection Factor (UPF) label. A UPF of 50 blocks about 98% of the sun’s UV rays.
Skin care
- People with diabetes should practice good skin care to prevent infections and promote healing. Regularly using fragrance-free moisturizers, especially on feet and hands, helps prevent cracks which can minimize the risk of infections.
- Harsh soaps can strip away natural oils, worsening dry skin. Using gentle cleansers and avoiding excessive washing also helps maintain healthy skin.
- Examine your skin regularly and look for any changes in your skin, such as new moles or growths, or changes in the size, shape, or color of existing moles. If you notice any changes, see your doctor right away.
Foot care (even at the pool!)
- While the cool sand or pool deck might tempt you to ditch your shoes on summer days, be aware of potential hazards. Bare feet can easily step on sharp objects hidden in the sand or sustain burns on hot pavement.
- To keep your feet safe, prioritize daily inspections for cuts, blisters, and calluses. Early detection allows for prompt treatment and preventing infections.
- Regularly moisturizing your feet and wearing comfortable, well-ventilated shoes, even at the beach or pool is key.
Eye protection
- Always wear sunglasses when in the sun. Look for sunglasses that have a label that says they block 100% of UVA and UVB rays.
Blood sugar management
- Monitor blood sugar levels more frequently, especially during sun exposure.
- Stay hydrated to avoid dehydration, which can worsen blood sugar control.
- Be prepared to treat low blood sugar (hypoglycemia) with fast-acting carbohydrates like juice, fruit snacks or dried fruit.
Medications
- Certain medications can increase sun sensitivity. Make sure to discuss sun protection and how your medications may impact your sun sensitivity with your doctor or pharmacist.
- Some medications such as insulin may lose some effectiveness when exposed to extreme temperatures. The longer the exposure to extreme temperatures, the less effective the insulin becomes. This can result in loss of blood glucose control over time. Keep insulin away from direct heat and out of direct sunlight and store between 59°F and 86°F.
Hydration
- Being outside in the sunlight can cause dehydration, which can make blood sugar harder to control.
- Ensure you are drinking plenty of fluids, especially if exercising outdoors on a sunny day. The National Academy of Medicine recommends 9 cups of water daily for women and 13 cups daily for men. A good rule of thumb is to listen to your body and drink when you feel thirsty.
- If you suspect you might be dehydrated, the best thing to do is to rehydrate as soon as possible with water or electrolyte-rich fluids such as SOS Daily Hydration. Always seek medical attention if you experience severe symptoms or dehydration doesn’t improve after rehydrating on your own.
In summary
In conclusion, sun safety is an absolute must for everyone, but it holds particular importance for those living with diabetes. The increased risk of skin complications, delayed healing and even potential impacts on blood sugar regulation require a proactive approach to sun protection.
By incorporating sunscreen, protective clothing, shade seeking and proper skin care into your routine, you can significantly reduce these risks and enjoy the outdoors safely.
Remember, sun protection is a team effort. Don’t hesitate to discuss your individual needs and the best sun safety strategies with your doctor at your next appointment.
Featured Products


The post The Importance of Sun Protection for People Living With Diabetes first appeared on The Upside by Vitacost.com.


