During cold and flu season, taking simple steps like washing your hands, keeping your home clean and supporting your immune system can help you avoid getting sick. But there’s may be another weapon you can add to your “sick season” arsenal: supporting your gut health.
Flu, the common cold and gut health
Sounds weird, right? Your gut is pretty far away from your nose and lungs. But the two “talk” to each other all the time — and share some common immune functions and structures. That means one can influence the other, which may impact your risk of getting sick and affect how your body responds if you do come down with a cold or the flu.
The “gut-lung” axis in cold and flu
Your gut and lungs are lined with tissue called mucosa. The surfaces of cells in this tissue have receptors for proteins that immune cells produce to communicate with other cells. Both the gut and lung mucosa have some of the same types of receptors, so when you have an infection like a cold or the flu, immune cells can travel through your bloodstream from your gut to your lungs to help fight it off.
These immune cells learn their job in the GALT—gut-associated lymphoid tissue— a collection of specialized cells in the gut mucosa. The GALT trains immune cells to recognize patterns associated with pathogens and home in on them. Once they migrate to the site of an infection, the trained cells activate other immune cells to mount an attack.
But these interactions aren’t always beneficial. Inflammation in your lungs can disrupt the balance of microbes in your gut and disturbances in your gut may make lung inflammation worse. These back-and-forth effects may impact how your immune system responds to infections.
Immunity, the gut and the flu
Take, for example, a case of the flu. When you first start to come down with the virus, your gut prompts your body to ramp up production of immune cells called T helper (Th) cells. Your gut microbiome plays a role in helping these immune cells mature and specialize. When Th cells like Th1 and Th17 reach the lungs, they release pro-inflammatory compounds called cytokines to support immune cells, attack the virus and clear the infection.
Cytokines can move from the lungs to the gut while you’re sick, which may decrease beneficial bacteria like Lachnospira-ceae, Lactobacillaceae and Bifidobacteriaceae and promote the growth of gut microbes that can be pathogenic like E._coli, Helicobacter_hepaticus and Clostridium_perfringens.
The increase in pathogens can trigger a pro-inflammatory cycle that damages the protective barrier lining your gut, makes the gut “leaky,” and contributes to inflammation elsewhere in your body. Being in this inflammatory state can make you more susceptible to getting a secondary infection like E. coli or bacterial pneumonia during or right after the flu.
Gut microbes and the common cold
But what about upper respiratory infections like the common cold? Even though the gut-lung axis isn’t involved, microbial balance may still be important. Having more pathogens like Escherichia, Shigella, Turicibacter, Holdemanella or Actinomyces may promote inflammation and contribute to barrier damage. This can disrupt the balance between gut immunity and immune function in other body systems and increase your risk of coming down with a cold.
But if your gut has more beneficial bacteria—such as Gordonibacter, Rhodospirillaceae or Actinobacteria—you could be protected against infection. These microbes may support a healthy microbiome and stimulate the production of anti-inflammatory compounds. Even more important, though, may be their production of short-chain fatty acids (SCFAs), which have been shown to support immunity throughout the body.
Support gut health to promote immunity
Interactions between SCFAs and your immune system appear to be one of the main ways your gut “communicates” with your lungs, so supporting gut microbes that make SCFAs could help maintain healthy immune function during cold and flu season.
High-fiber foods to promote SCFAs
How exactly do SCFAs regulate immunity? Research suggests that these compounds may:
- Promote a healthier inflammatory response by regulating how many immune cells travel to the site of an infection and release cytokines
- Support the production of anti-inflammatory cytokines
- Maintain healthier levels of immune cells and and pro-inflammatory cytokines by regulating a protein called histone deacetylase (HDAC)
- Regulate how immune cells mature and develop pro-inflammatory responses
- Modulate immune responses by interacting with g protein-coupled receptors, a type of receptor found on the surface of immune cells
- Support healthy barrier function to regulate inflammation
Supporting SCFA production can be as simple as changing your diet. The gut microbes that make SCFAs love fiber from whole and minimally processed foods like whole grains, beans, vegetables, fruits, nuts and seeds—which are abundant in diets like the Mediterranean diet and the MAC diet.
Many fiber-rich foods are also high in compounds called polyphenols. Polyphenols may also promote gut health and immunity by:
- Supporting and maintaining a healthy gut barrier
- Regulating a pro-inflammatory protein called nuclear factor kappa beta (NF-κB)
- Maintaining healthy antioxidant levels and anti-inflammatory antioxidant activity
To increase polyphenols in your diet, eat more colorful fruits and vegetables like apples, grapes, berries, tomatoes and red and yellow peppers. Spices like turmeric and beverages like green tea are also good sources. (And dark chocolate, so go ahead and enjoy a square for dessert!)
Natural solutions to promote gut health
If you do get a cold or flu that leaves your gut feeling a little off, these supplements may help you get back on track:
- L-glutamine promotes healthy cells for a strong gut barrier†
- Zinc carnosine supports protein production and cell division for a healthy gut membrane†
- Deglycyrrhizinated licorice (DGL) may support the healthy production of mucus that protects the gut lining†
- Vitamins A and D may help support healthy barrier permeability and support healthy diversity in the gut microbiome†
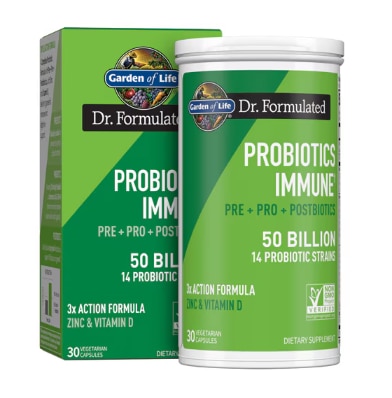
Probiotics for immune function?
It’s unclear whether probiotics belong on the list of supplements to promote healthy immune function in cold and flu season. In animal and human studies, probiotics appear to promote antiviral cytokines, promote a healthy inflammatory response and support healthy barrier function, which may be why probiotics like Lactobacillus, Bifidobacterium and Lactococcus appear to support healthy respiratory function. But results aren’t consistent across research, and the outcomes aren’t always significant.†
Even with a high-fiber diet and gut-supporting supplements, It’s hard to completely avoid getting a cold or flu once the season for respiratory infections arrives. But it doesn’t hurt to do all you can to stay healthy—including maintaining good gut health to promote strong immunity.†
†These statements have not been approved by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent disease.
Featured Products


The post Does Getting a Cold or the Flu Affect Your Gut Health? first appeared on The Upside by Vitacost.com.

