No matter where you go, you come in contact with mold. It’s in the air and in the soil, in your bathroom and under your kitchen sink.
And, sometimes, in your food.
As food molds grow, they produce compounds called mycotoxins, which have the potential to disrupt your gut health and make you sick.
Food molds and mycotoxins
Molds that produce mycotoxins aren’t always as obvious as those fuzzy blobs on the bread ends you forgot about in the back of your fridge. They’re typically found in food and feed crops that aren’t processed, stored or handled correctly or are exposed to damp conditions. It’s estimated that mycotoxins may contaminate up to 80% of food crops around the world.
Common mycotoxins and their sources include:
- Aflatoxin: peanuts, corn, tree nuts, small grains like rice
- Deoxynivalenol: bread, noodles, beer, popcorn and grains like wheat, corn, oats and barley
- Fumonisins: corn and sometimes other grains
- Paulin: fruit, grains, nuts, cheese, apples and apple juice made from contaminated apples
- Ochratoxin A: coffee, grapes, wine and grains like wheat, rye, oats and barley
- T-2 and HT-2 toxins: grains, including wheat, rye and barley
- Zearalenone: corn, oats, wheat, sorghum, rice and other grains
You can be exposed to mycotoxins by eating these foods or products made from animals that ate contaminated feed.
Do mycotoxins in food hurt your gut?
Chronic mycotoxin exposure may cause long-term health effects, which may be influenced by how these compounds impact your gut’s microbiome and tissue.
Mycotoxins may damage your gut’s lining
Your gut is lined with a layer of cells called epithelial cells held tightly together by junction proteins and covered with a barrier of mucus. The proteins ensure that food and microbes stay in the gut, and the mucus lubricates and protects your gut tissues.
Mycotoxins like ochratoxin and zearalenone may damage this barrier by reducing the production of junction proteins and mucus. They may also promote inflammation by activating gut immunity and increasing the levels of pro-inflammatory compounds called cytokines, which can damage or destroy the epithelial cells lining your gut.
When your gut’s lining is damaged, food particles, bacteria and toxins can “leak” between cells into your bloodstream and trigger immune responses in other parts of your body, which may contribute to inflammatory disorders and autoimmunity.
Mycotoxins may disrupt gut microbiome balance
A balanced microbiome is also essential to keeping your gut healthy. But mycotoxin exposure can affect microbial balance at every level from phylum to species. Animal studies on mycotoxin exposure have shown changes in the microbiome’s structure and diversity that include:
- Fewer beneficial bacteria like Lactobacillus
- More pathogens like Mycoplasma
- A shift in the ratio between Firmicutes and Bacteroidetes
Decreased diversity and microbials imbalances in the gut have been linked to a variety of health problems, including cardiovascular disease, autoimmune disorders and inflammatory bowel disease (IBD).
Can your gut microbiome protect against mycotoxins?
But mycotoxins may not be as much of a problem if you already have a healthy population of microbes in your gut. Beneficial gut bacteria, including lactic acid bacteria like Lactobacillus, Mycobacterium, Rhodococcus, may be able to convert mycotoxins into less-toxic or non-toxic compounds that your body can eliminate safely. In vitro studies show that some bacteria can reduce the concentration of mycotoxins by up to 98%. Bacteria and yeasts may also remove mycotoxins from the gut environment by binding them to compounds in their cell walls.†
A few probiotic species have been tested for their potential to stimulate mycotoxin removal. Some studies show that yeasts in the Saccharomyces genus and bacteria like Lactobacillus rhamnosus, Lactobacillus plantarum and Lactobacillus pentosus may be able to break down or bind these toxic compounds. But more research is needed to understand how effective these probiotics are at regulating mycotoxin levels in humans.†
How to protect your gut from mold and mycotoxins
The Joint FAO/WHO Expert Committee on Food Additives (JECFA) has established safe maximum daily intake levels for mycotoxins from food. Known as health-based guidance values (HBGV), these numbers represent the highest level of each mycotoxin you can be exposed to per day over a lifetime without any noticeable impact on your health. Additionally, the FDA monitors mycotoxin levels to minimize the risk of contaminated products entering the food supply.
You can also take steps to prevent mold and mycotoxins from forming on foods in your home. To reduce your exposure:
- Inspect dry goods like grains, nuts and dried fruit. Throw away anything that looks moldy, discolored or shriveled.
- Inspect the food in your fridge frequently for mold. Throw out fresh, packaged or prepared foods that have visible mold.
- Freeze uneaten leftovers within three to four days.
- Don’t try to trim or skim molds off soft and liquid foods. Mold spreads more easily through these foods and may not always be visible.
- Store dry goods in airtight containers in a cool, dry place.
- Transfer packaged foods like cookies, chips and crackers into airtight containers for storage.
- Clean fridge drawers, bread boxes and other food storage spaces often.
- Eat a diverse diet to support a healthy microbiome.
†These statements have not been approved by the Food and Drug Administration. These products are not intended to diagnose, treat, cure or prevent disease.
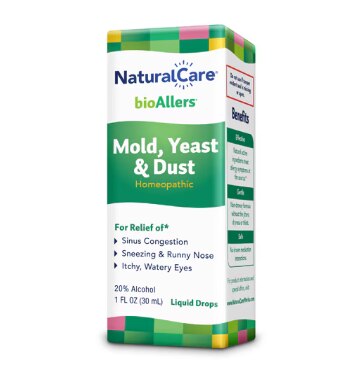
Featured Products


The post Is Hidden Mold in Everyday Foods Hurting Your Gut Microbiome? first appeared on The Upside by Vitacost.com.

